From basic care to prevent Covid-19 during pregnancy to the risks of self-medication with substances such as Ivermectin, recently adopted in Natal to combat the disease. See, below, the highlights of the interview with the general director of the Santos Dumont Institute (ISD) and specialist in fetal medicine, Reginaldo Freitas Júnior, on live “Guidelines for pregnant and postpartum women in times of Covid-19”, promoted by Guia Viver Bem (@guiaviverbem) on June 10th.
Reginaldo Freitas Júnior has a doctorate and master's degree in Medical Sciences from the Faculty of Medicine of Ribeirão Preto at the University of São Paulo (USP). He is also a specialist in Fetal Medicine at the Brazilian Federation of Gynecology and Obstetrics Associations (FEBRASGO), has a medical residency in gynecology and obstetrics at Maternidade Escola Januário Cicco (UFRN) and is an associate professor at the Department of Tocogynecology at UFRN. He is the advisor for the Professional Master's Degree in Health Education (UFRN) and the Master's degree in Neuroengineering from the Edmond and Lily Safra International Institute of Neurosciences (IIN-ELS/ ISD), in addition to being National Instructor of the Zero Maternal Death from Postpartum Hemorrhage Strategy of the Pan American Health Organization/World Health Organization (PAHO/WHO), together with the Ministry of Health. He has been general director of ISD since 2018.
In the live broadcast, in an interview with journalist Juliana Garcia with questions also from followers of Guia Viver Bem on Instagram, he emphasizes that “you should not suspend prenatal care, or avoid prenatal consultations due to the pandemic” and further responds to questions about the danger of inappropriate use of face shields in the maternity ward, about the possibility of transmission of Covid-19 from mother to baby through the placenta and about childbirth in the current context. Check out the main points below and watch the conversation in full in the video below, also available on ISD channel on YouTube.
INTERVIEW: Reginaldo Freitas Júnior
What do pregnant women need to be guided by during this pandemic, so that they get through this phase, the time of birth arrives and everything is fine?
The first point to be highlighted is that we are still living in a period of many more questions about this correlation between Covid-19 and pregnancy than concrete answers. So, much of what we have adopted as conduct and guidance has to do with our previous experience with other respiratory-transmitted viruses, such as H1N1, and experiences with other infections that could pass from mother to baby, such as the case of Zika virus infection. In Covid-19, many questions are still unanswered. At the beginning of the pandemic, considering the experiences of other countries that had already experienced the pandemic before Brazil, pregnant women were initially classified as not being a higher risk group. And, looking in the rear view mirror, we realize that in a way this brought an additional risk. Not that pregnant women should panic because they are pregnant and we are living through a pandemic, the idea is not to scare them. That's all they don't need. However, as pregnancy changes many things in a woman's body, including the immune system, it is necessary for pregnant women to be understood as a group that deserves special attention and that deserves more care during pregnancy. Another thing that I think is important to highlight is that many symptoms that are typical of pregnancy are capable of confusing pregnant women in relation to other diseases. And Covid-19 is no different. So, pregnant women may experience more tiredness, some difficulty breathing, coughing, the issue of gastroesophageal reflux during pregnancy, which is very common and causes coughing, hoarseness and this often leaves women unsure about whether it is or not the manifestation of a disease that is so frightening. So a first point to highlight is: we know less than we would like and because of the special fragility of pregnancy, this special condition of being pregnant, we need to be seen as a group that It deserves very special care.
What are the main precautions at this time when it comes to going to prenatal care, another appointment or if the woman needs to go out to do something else?
It is essential to highlight that prenatal care, even for pregnant women who do not have other complications, which is what we call habitual risk prenatal care, needs to be seen as an essential service. And it must be continued. We should not suspend prenatal care, or avoid prenatal consultations due to the pandemic. Obviously this can be adapted. So during this period we have recommended that the first trimester of pregnancy, up to 14 weeks, and the last trimester of pregnancy, from 28 weeks onwards, are the priority moments for face-to-face consultations, where it is very important that the pregnant woman is really in the doctor's office, for her to be examined, for her to be seen, and for this care to take place in person. In the middle of pregnancy, in the second trimester, which is a period that tends to be calmer, we can use resources such as telemedicine. Today, for example, WhatsApp has actually ended up becoming a care tool, even regulated by the Federal Council of Medicine, which means that there is permission for this to happen. But the first point is: maintain prenatal care, prioritizing consultations in the first and third trimesters. In the second trimester, appointments can be spaced out further, exams can be spaced out further so that this pregnant woman really stays at home, so that she really complies with the only effectively proven measure (to date) to prevent contamination, which is social isolation , and that for this moment of greater distance from the health service, from the doctor's office, these remote care tools, such as telemedicine, WhatsApp, virtual consultations, can be used. But prenatal care should not be suspended. It should not be discontinued due to the pandemic.
In this last trimester, as it gets closer to childbirth, I imagine that pregnant women are afraid of going to the hospital, of becoming infected, or (of this happening to) the baby when it is born, as we have already seen cases. So what is the care right now?
Pregnant women should really take extra care when going out. Wearing a mask is essential in all these environments. Despite being a respiratory-transmitted virus, the whole world has already proven that the main source of contamination is in our hands. So, every time it is really necessary to leave the house for a medical appointment, for an examination, in a situation where this exit is essential, take care to wash your hands, protect your eyes, the mucous membrane of the nose, the mucous membrane of the mouth, it needs to be permanent. In the third trimester, trips will be more frequent and so will the need for this care. In relation to childbirth, we have been careful to advise health services that the births of symptomatic pregnant women need to take place in different environments. Therefore, it is very important that pregnant women pay attention to whether the services that provide birth assistance have organized these flows. This is a patient safety issue. It's a matter of necessity even now. So the maternity hospitals, the services that serve women at the end of pregnancy in Rio Grande do Norte, at least, they were guided – the State Department of Public Health itself released a document in which we had the pleasure of also participating – guiding the organization of these flows, (guiding) that from the entry point of these services, screening already takes place for pregnant women who have symptoms, or who have a fever, and that from then on, the entire path of care in the services is a path different. The delivery room itself, we have advised that it be a specifically separate delivery room for pregnant women who have symptoms. Even if that pregnant woman, at that moment, has not yet been tested or we have not yet obtained confirmation, the service must prepare to care for the symptomatic pregnant woman in another way within the institution to avoid contamination at the time of birth.
Should a pregnant woman undergo serology even if she has no symptoms? Is this information important for pregnant women?
If she has no symptoms, the indication for serology would be more related to exposure (to the risk of the disease). Of course, depending on the service this pregnant woman is in, the access she has to testing, this can be adapted to the reality of each situation. But testing for Covid-19 is not part of the routine of prenatal exams. So the way women are tested for HIV, for syphilis, for hepatitis, they are not being tested for Covid-19 indiscriminately. We are testing in specific exposure situations and evaluating case by case.
Is it better to catch Covid at the beginning or end of pregnancy?
The best thing is not to catch Covid. But this question is super important. Because we still do not have sufficient data on exposure to Covid-19 in the first trimester of pregnancy. We still don't know how to answer, for example, whether Covid is capable of causing malformations like Zika did, like toxoplasmosis causes, like rubella causes, like syphilis causes. We don't have that answer yet. But there is new information. Until the last week of May, the world still did not have proof that the new coronavirus had passed through the placental barrier. We had cases in China, we had cases in Italy, but these cases did not prove the virus passed through the placenta and reached the baby. And then unfortunately that changed. A French publication, from the last week of May, in the magazine Nature, probably documents the first case of vertical transmission of Covid-19 from mother to baby. It was a woman in her first pregnancy, a 23-year-old woman, who gave birth to a 35-week-old baby prematurely, and before the baby was born, a sample of amniotic fluid was taken. In this sample, the baby had no contact with the external environment, he had not had contact with his mother yet, that is, he had not become contaminated in the environment and it was possible to identify the RNA of this virus both in the amniotic fluid and in the cord blood and in the placenta. So this is probably the first case. We call this vertical transmission. It is the first case probably documented and this opens another window. So if we now know that the virus can pass from mother to baby, another range of possibilities arises, from the possibility of causing some type of malformation or other problem. The newborn babies who became infected, most of them had the somewhat more common symptoms of the disease and most of these babies came out fine. This baby with vertical transmission was discharged well. But the first trimester of pregnancy is always the period of pregnancy that concerns us most, because it is the period when the baby is forming, when all the organs are being built, and when external agents in general can disrupt this organogenesis and this formation of the baby. So unfortunately I think The first trimester is still the most worrying for the pregnant woman, although it may seem curious, but for women's health, it seems that the period after childbirth, which we call puerperium, the 42 days after birth, has been the period where pregnant women have most experienced complications from Covid-19. And that really catches our attention. The majority of pregnant women, women and maternal deaths that occurred due to Covid-19 occurred during the postpartum period and this is a very important warning for all of us, health care providers and for all of us patients and citizens. So the period after birth deserves very special attention from families, people who care for pregnant women, the pregnant woman herself in relation to care and those who care for her, health professionals.
Is it necessary to use a face shield in the maternity ward?
The face shield is more specific protection for healthcare professionals, for people exposed to aerosols. So the face shield alone does not protect. It needs to be used together with the (surgical) mask, with the glasses and with the hat, and in the maternity hospital itself I have the impression that the (fabric) mask is enough. I think that from the point of view of contact with the baby, I think even for the comfort of the pregnant woman, it seems paradoxical, but improperly used personal protective equipment can bring as much risk as not using it. So the face shield is individual, it needs specific cleaning after each use and one thing that concerns us when we use personal protective equipment like this is the feeling of safety that it can often bring to those who are using it. 'Ah, I'm wearing a face shield so I can go out, I'm wearing a face shield, I can talk without a mask… I can remove the face shield with my hand (touching the surface) and then put my hand on my nose or mouth '. What we have advised is the use of a (fabric) mask as protection in maternity, childbirth and breastfeeding, for example.
Many people are using Ivermectin… Would you recommend it to pregnant women?
We have never studied this drug in pregnant women. We only have in vitro studies, studies carried out either with cell cultures or with animal species, but it has never been tested for use in pregnancy or in higher doses. So naturally, historically, we did not and do not use ivermectin during pregnancy, especially in the first trimester. Remember that it is a drug that is toxic to the liver. And it is a drug that can cross the placental barrier, so it can be toxic to the mother's liver and toxic to the baby's liver. So we are very careful to clarify that at the moment we are not confident enough to recommend the use of ivermectin during pregnancy. Using it can also bring this feeling of security, of 'I can do it because I'm taking ivermectin' and this is worrying and deserves warning. From everything we have studied and proven, these are general, simpler measures such as hand washing, avoiding contact, coughing etiquette, sneezing etiquette, truly protecting other people who have contamination from contamination. proved to be more effective. I hope that very soon we will have an alternative that brings true security to all of us.
_______________________________________________________
SEE TOO
The warning from the ISD general director regarding the risks of self-medication with Ivermectin during pregnancy was highlighted recently in the printed and online versions of Tribuna do Norte and in reports from RN TV 2nd edition and Bom Dia RN, from InterTV Cabugi (from 13 minutes and 34 in the RN TV edition of June 11th. Click here to see).
_______________________________________________________
Would a pregnant woman catching Covid be fatal for the baby?
We still don't have this information as to whether it can be fatal for the baby or not. This is something that we have still studied and we are still looking for this answer.
What are the risks for this pregnant woman who is infected by Covid?
Regarding pregnant women with Covid, one thing that has worried us a lot is that it seems that this virus has a very special effect on the blood clotting system. We call this system hemostasis. The pregnant woman already has the blood clotting system diverted to the procoagulant. This is a protective mechanism to prevent the pregnant woman from bleeding too much during childbirth, to prevent her from dying from bleeding. Nature did this to all mammals. When all female mammals become pregnant, the blood clotting system becomes clotted more easily. And we have noticed that pregnant women with Covid have had more thrombotic complications than the general population. So, one thing we have been careful about is alerting to these signs, classifying these pregnant women according to the risk of thromboembolic phenomena, for example in relation to the body mass index, the index that measures the relationship between weight and height, the presence of varicose veins, the presence of a history of thrombotic phenomena, the presence of a family history of blood clotting diseases, a personal history of thrombophilia. So in these pregnant women we have taken very special care with blood clotting, including in some situations using prophylactic, preventive medications to prevent these phenomena from happening. Another important thing is the attention that pregnant women must pay to these symptoms that can be confused with pregnancy symptoms. During pregnancy specifically, shortness of breath, cough, malaise, fever, really demand health care, so it is important that in these real situations she seeks the health service to be evaluated, so that we do not underestimate the disease. , so we don't underestimate the risks.
Is early birth recommended for women diagnosed with Covid?
The mode of delivery and the time of delivery are situations that will depend greatly on the clinical condition of the pregnant woman. Early birth will be indicated when (the disease) compromises the continuity of the pregnancy, compromises the pregnant woman's health or puts the baby's survival at risk. So, in some situations, the maternal condition is so serious that we need to interrupt the pregnancy in order to guarantee better care for the pregnant woman. So in this situation, early birth is indicated. Or because the main complications of Covid in relation to the baby are related to the lack of oxygenation of the blood due to the work of the placenta. In these situations, we would recommend (early) birth for the baby's health. But indicating premature termination of pregnancy simply because you have Covid is not something that guarantees safety for either the mother or the baby.
Postpartum – What care should this mother follow? Do I have to wear a mask? follow all that hand hygiene protocol?
You have to wear a mask, you have to wash your hands every time you touch the baby, change the baby, breastfeed the baby. It is very important that this is assumed by these pregnant women as a habit. These precautions really need a lot of attention. Help from someone who is healthy with breastfeeding is also important. What is still controversial – some people advise, others don't – is the issue of breast hygiene. It is not an absolute consensus. Historically, we didn't need to clean our breasts for breastfeeding. In the context of the pandemic, these opinions differ. So we can still have new chapters of this story. In general, some services have advised breast hygiene before breastfeeding. But I repeat that this is not consensual and we still do not have strong evidence to recommend this as a certainty.
Are there tests that can identify the risk of thrombosis close to birth or risks to the baby?
There are blood tests that help us with this (to identify the risk of thrombosis) and can be done. Regarding complications to the baby's health, malfunctioning of the placenta, and poor oxygenation of the baby, there is an exam called fetal hemodynamic profile, which we do using ultrasound, with another tool called doppler. It is another ultrasound tool that can very early suspect babies who are at greater risk of having a drop in blood oxygenation due to placental malfunction.
Pregnant patient diagnosed with Covid.. would it be interesting to increase the number of ultrasounds to monitor this pregnancy?
We have been doing this mainly at the end of pregnancy. Obviously, this will depend a lot on this pregnant woman's access, the reality where she is, and what tools for assessing fetal vitality are available in the context where she is inserted. But we have been monitoring, according to the reality of each service and each social context, we have been monitoring pregnant women much more at the end of their pregnancy with Covid.
I imagine, doctor, what your routine is like. On one side there are these pregnant women who have all this assistance and on the other there are those who don't. I see it through the Santos Dumont Institute and all that research you did regarding maternal mortality associated with Covid. They are very different realities, aren't they?
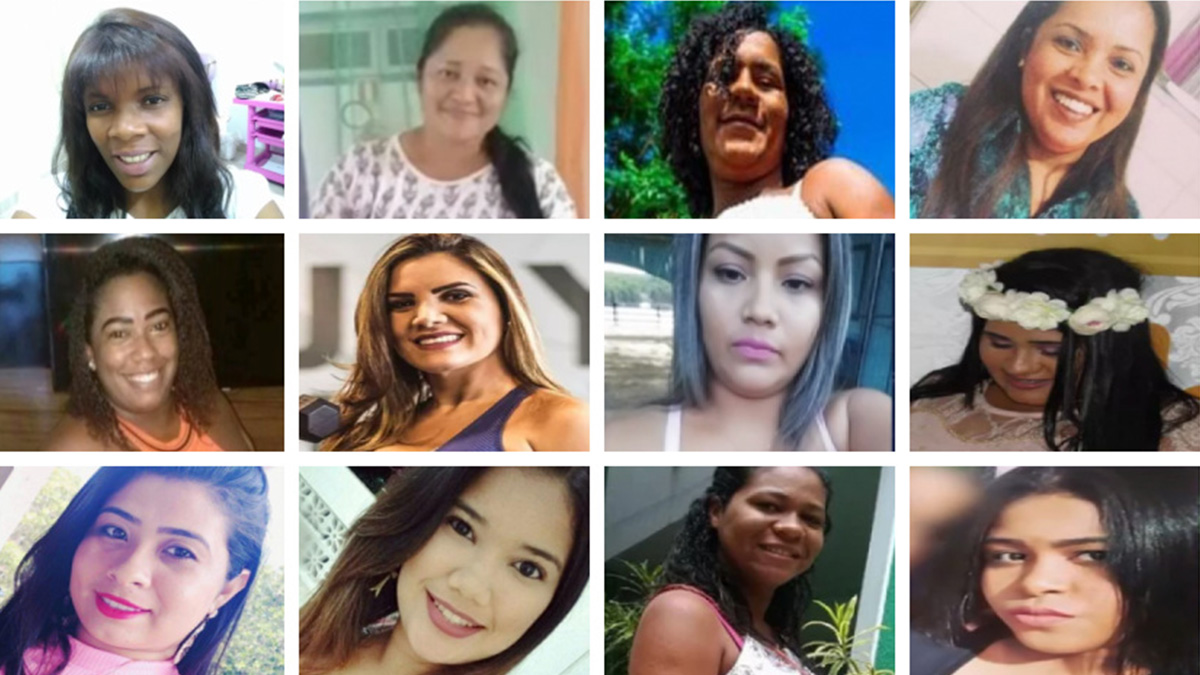
They are. This is something that Covid-19 is bringing to light in a way. Our country is experiencing a very big paradox. Most of our women have babies in hospitals, they are cared for by doctors and nurses, but the country still has very high numbers of women who die due to complications during pregnancy, childbirth and the postpartum period, much higher than the World Organization. of Health recommends, and far above what is acceptable for this reality, giving birth in a hospital. So, in fact, between the lines, what we read is that there is an issue closely related to the quality of this assistance and these women's access to this assistance. In this survey that you mention, it is not official data, but together with our communications department we mapped all the news about deaths of pregnant women, or during this period of pregnancy, childbirth and the postpartum period reported by the media. Because historically, these women have always become statistics before becoming news. Many became statistics and never made the news. And this moment we are experiencing with Covid-19 has curiously done the opposite. In two months of media coverage in Brazil and around the world, we had more news about maternal deaths published in the media than we have had in a decade. And unfortunately most of this news is related to our country. So 51.8% of these news stories were from Brazilian women. And countries that had a higher total number of deaths from Covid than ours did not have this same experience due to pregnancy, childbirth and the postpartum period. So, unfortunately, what is happening is that Covid is shining a light on a problem that is historic in our country, which needs to be faced by each one of us because we have not really been a guarantor of the right to safe motherhood.
KNOW MORE
Click on the image to learn more about the ISD survey in the report "Brazil has more maternal deaths associated with Covid-19 than 8 countries combined". The survey is part of a series of publications by the Institute focused on the health of pregnant or postpartum women during the pandemic. All content can be viewed at https://www.institutosantosdumont.org.br/materiais-educativos-covid-19/.
Text: Renata Moura / Ascom – ISD
Communication Office
comunicacao@isd.org.br
(84) 99416-1880
Santos Dumont Institute (ISD)
It is a Social Organization linked to the Ministry of Education (MEC) and includes the Edmond and Lily Safra International Institute of Neurosciences and the Anita Garibaldi Health Education and Research Center, both in Macaíba. ISD's mission is to promote education for life, forming citizens through integrated teaching, research and extension actions, in addition to contributing to a fairer and more humane transformation of Brazilian social reality.